What’s the big deal about wet cough?
A wet cough in a child for more than four weeks could indicate infection in the lungs. The wet cough is caused by mucus in the airway. The mucus becomes infected with bacteria and causes airway inflammation that can progress to permanent lung damage known as bronchiectasis.
Bronchiectasis is a chronic respiratory disease that can cause early death and has been called an ‘orphan’ or ‘neglected’ disease, in part due to its low prevalence in western countries. However, bronchiectasis is prevalent in Australian Indigenous people. The disparity between Indigenous and non-Indigenous patients with bronchiectasis is particularly marked. In the Kimberley region of Australia, the median age at death for Indigenous adults hospitalised with bronchiectasis was 33 years.
Children are not born with bronchiectasis; rather it develops over time. The longer the duration of wet cough in a child, the more extensive the lung damage can be. In young children, bronchiectasis can occur when the lungs’ defenses are overwhelmed by infections like pneumonia. Air pollution, dust and smoke can also contribute to lung infection. Under-recognition and undertreatment of chronic wet cough can also lead to bronchiectasis. However, damage can be halted, limited or reversed if chronic wet cough is detected and managed early.
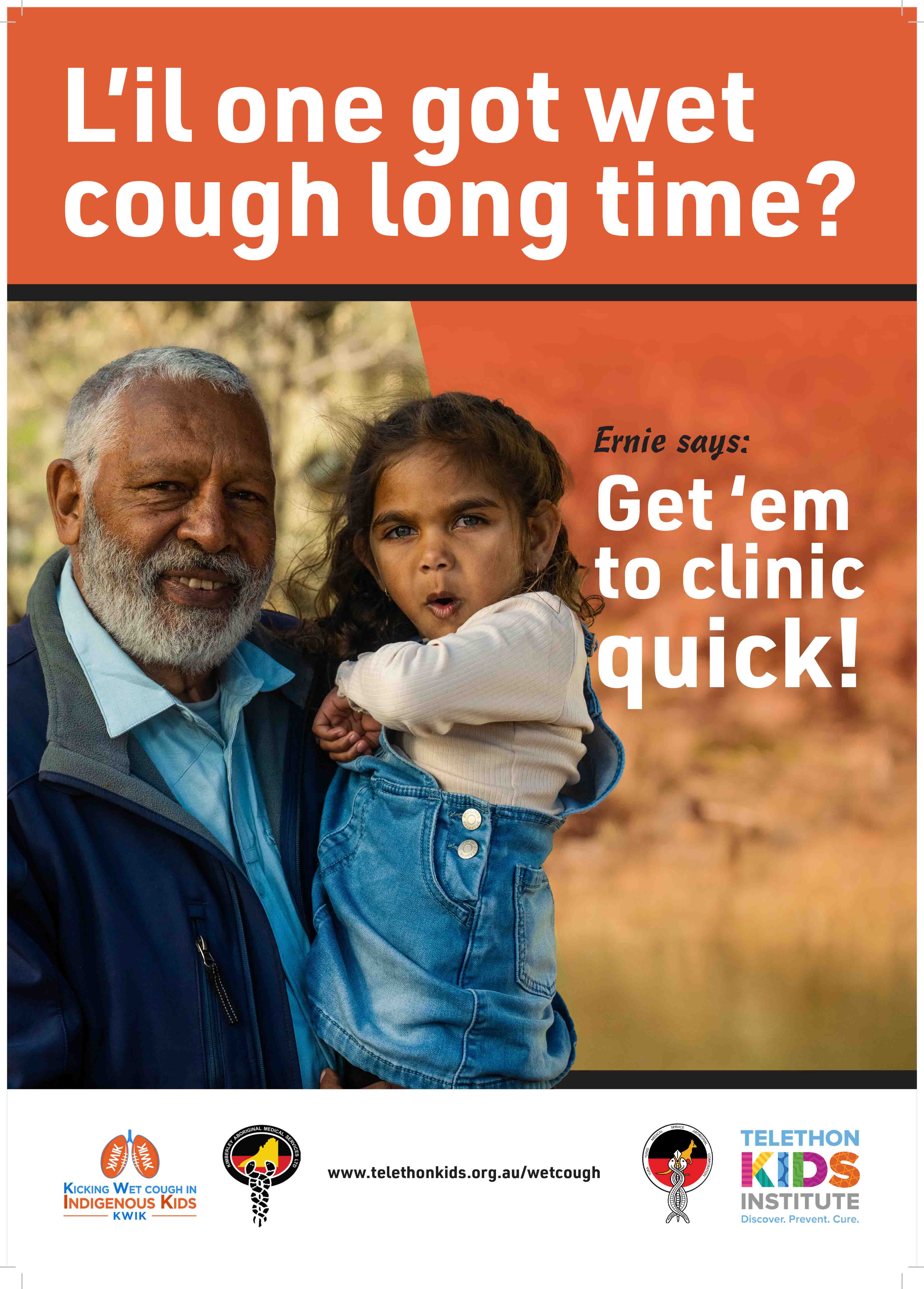
One of the biggest problems in managing bronchiectasis in Indigenous people is that diagnosis is often delayed by years and decades. Early detection is difficult because children may appear well. Often the only early sign is a chronic wet cough, which people do not always ‘hear’ because it can be so prevalent it can become normalised. If cough is normalised (i.e. considered to be normal), families may put off seeking medical help.
Our own research in the Kimberley has shown that families normalised chronic wet cough and did not realise it required medical review. However, families are highly receptive to health information and told us they would seek help if they knew about the link between chronic wet cough and bronchiectasis.
Low clinical suspicion by health practitioners can also delay diagnosis. National management guidelines were not developed until 2006 and are not widely known by health practitioners. Furthermore, bronchiectasis in children has not always been on health professional curriculums. In fact, the problem of chronic wet cough and bronchiectasis in Aboriginal children appears to still be widely under recognized.
What are we doing about the problem?
At The Kids, we believe that the burden of chronic lung disease in Aboriginal adults can be reduced if early lung disease is managed effectively in children. We are researching ways to help improve the management of chronic wet cough in childhood to help reduce the burden of chronic lung disease in adults
We are conducting research in a number of Aboriginal communities in the Kimberley. Our research is being done in partnership with local Aboriginal and other Medical Service providers, and community members.
Our objectives are to:
- Accurately determine the prevalence of chronic wet cough in Aboriginal children in the Kimberley
- Improve healthcare of Aboriginal children with chronic wet cough through developing culturally sensitive and sustainable solutions for early detection; accurate diagnosis; and timely treatment of chronic wet cough.
Predicted benefits and outcomes
The proposed projects will create transformational change in the lung health of Aboriginal children by:
- Focusing attention to an under recognised problem by being the first to accurately determine the prevalence of chronic wet cough to quantify disease
- Creating widespread community awareness of the importance of lung health and chronic wet cough. We will implement and test a culturally appropriate health information campaign about lung health and chronic wet cough in children
- Training health practitioners in the assessment and management of chronic wet cough according to national guidelines.
Listen to the Engaging effectively with Aboriginal parents about children’s lung health podcast.

