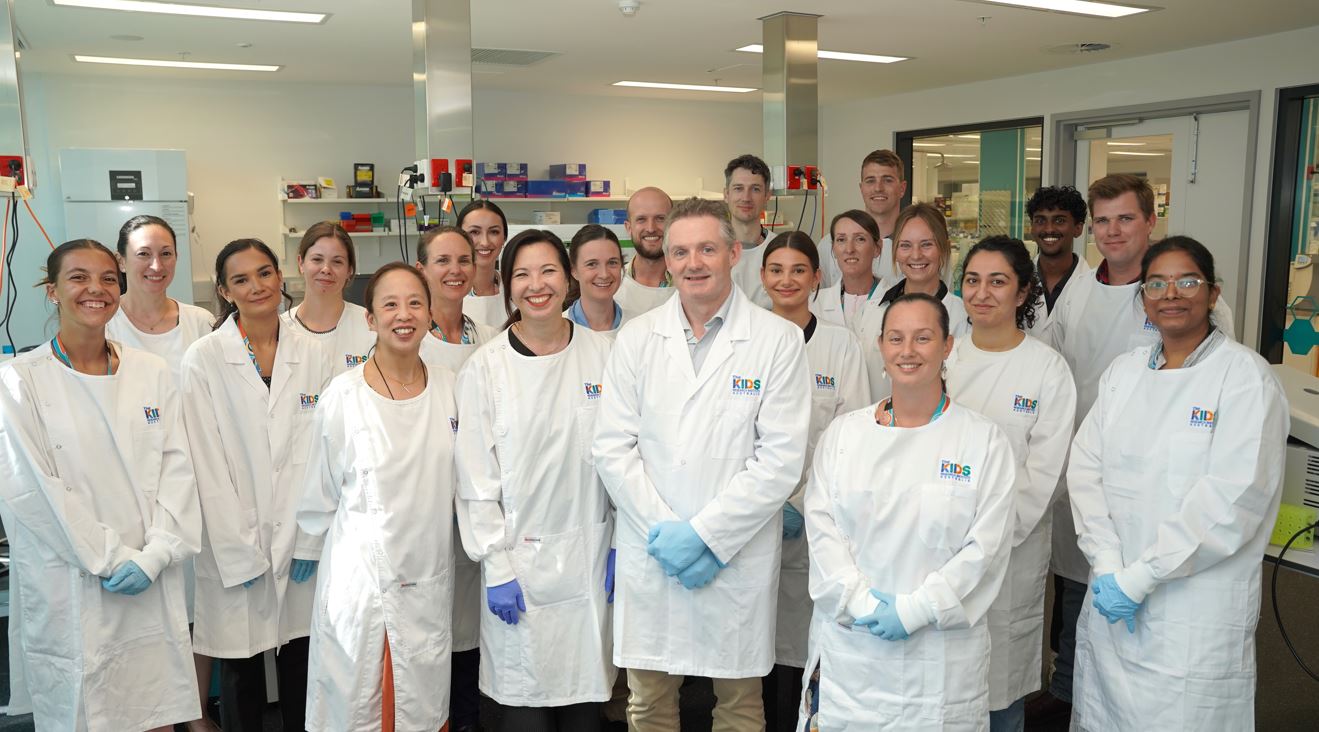
The Brain Tumour Research Laboratory was established in 2011, bringing together the clinic and the laboratory to advance research into childhood brain tumours.
The team is a collaborative group of researchers dedicated to improving our understanding of paediatric brain tumour biology and finding more effective treatments to improve survival rates and quality of life for patients.
The skills of our team members are diverse and include laboratory scientists from academia and industry, clinical oncologists and neuro-surgeons.
Each member of the team brings their unique and varied experience to tackle our research questions. Researchers perform basic and pre-clinical research aimed at identifying the best targets for new therapies and effective new treatments for clinical trials.
Moreover, we collaborate with others who bring valuable expertise. These include, but are not limited to, radiologists (clinical and pre-clinical models), medical physicists (imaging), chemists (drug screening), pharmacologists (pre-clinical testing) and bioinformaticians (large scale analyses of brain tumour genomics).
The team has established a strong national and international reputation and is recognised as being the largest research team in Australia primarily focused on paediatric brain tumours. The major goals of the group are intensely focused on improving the wellbeing of children with cancer.
With strong ties between The Kids and Perth Children's Hospital, the team knows what it takes to get a new treatment into the clinic and their research goals are sharply focused on providing the pre-clinical evidence required to form the basis of new clinical trials.
The overarching scientific goals of our team approach to improving outcomes for children with brain tumours are:
- Elucidate the molecular basis of different brain tumour types, including medulloblastoma and ependymoma among others, through the analysis of primary patient specimens
- Improve understanding of the molecular events contributing to these diseases, by analysing the impact of altered signalling pathway activity on the survival, proliferation, invasiveness and tumorigenicity of brain tumour cells
- Develop novel preclinical models of paediatric brain tumours by relevant targeted genetic mutations to provide systems in which to test new treatments
- Obtain and test new therapies in appropriate brain tumour models through collaboration with members of the WA Kids Cancer Centre, other academic partners, and industry groups
- Translate our findings into improved therapies and design of new clinical trials, which we achieve through national and international collaborations with clinical trials consortia such as Australian Children’s Cancer Trials (ACCT) and the Children’s Oncology Group (COG).
Team leader
BSc (Hons) PhD
Brainchild Fellow; Co-Head, Brain Tumour Research

MBChB FRACP PhD
Head of Paediatric and Adolescent Oncology and Haematology, Perth Children’s Hospital; Co-head, Brain Tumour Research Program, The Kids Research Institute Australia
Team members (17)

BMedRes (hons), PhD
Pirate Ship Research Fellow

BSc(Hons), PhD
Senior Postdoctoral Researcher and Research Project Manager
BSc (Hons), PhD
Senior Postdoctoral Researcher

BSc, MBSc, PhD

BSc (Hons), PhD

Dr Chris Butler
Postdoctoral Researcher

Dr Zahra Abbas
Postdoctoral Researcher

Hilary Hii
Research Officer

Brooke Carline
Research Assistant

Jacob Byrne
Research Assistant

Sally Larder
Research Assistant

Alex Monson
Research Assistant

Piyusha Johnson
Research Assistant

Josh Ninan
Research Assistant

Hetal Dholaria
Clinical Fellow (Research) and PhD Student

Brad McCarthy
Medical Student

Adam Byass
Medical Student
Brain Tumour Research projects
Featured projects
Developing and characterising juvenile models of aggressive paediatric brain cancers for the evaluation of novel immunotherapies.
While profound treatment responses have been realised using immunotherapy for some cancer types, this is yet to be seen for paediatric brain cancer patients.
Finding new, safer and targeted therapies for paediatric brain cancer that amplify responses to radiation therapy
Radiation therapy is an essential component of brain cancer treatment. However, the high doses currently required are extremely damaging to the growing brains and bodies of children.